Explore the nuances of CT Angiography (CTA) and MRI Angiography (MRA) in this comprehensive guide. Discover their distinct technologies, safety profiles, image qualities, and clinical applications, shedding light on the evolving landscape of vascular imaging and the potential impact of advanced technologies on diagnostic precision and patient care.
Medical imaging has revolutionized the way healthcare professionals diagnose and treat a wide range of conditions, especially those related to the vascular system. Two commonly used Medical imaging techniques for visualizing blood vessels are CT Angiography (CTA) and MRI Angiography (MRA). While both methods serve similar purposes, they employ distinct technologies and have unique advantages and considerations. In this comprehensive guide, we delve into the intricacies of CTA and MRA, exploring their principles, applications, benefits, and differences.
CT Angiography (CTA): Unveiling the Power of X-rays
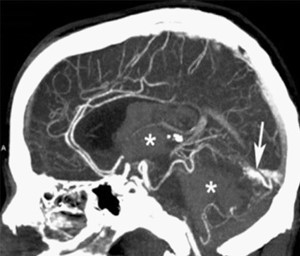
CT Angiography, often referred to as CTA, is a diagnostic imaging procedure that combines X-ray technology with the use of a contrast dye to visualize blood vessels in the body. The process begins with the patient lying on a motorized table that moves through a doughnut-shaped CT scanner. This scanner emits a series of X-ray beams from various angles, capturing detailed images of the internal structures, including blood vessels.
One of the primary advantages of CTA is its ability to produce high-resolution, three-dimensional images of blood vessels. This level of detail allows radiologists and clinicians to assess the vascular system for abnormalities such as aneurysms, stenosis (narrowing of blood vessels), arterial blockages, and vascular malformations. Additionally, CTA is known for its speed and efficiency, providing quick results that aid in prompt diagnosis and treatment planning.
The key principle behind CTA lies in the interaction between X-rays and the contrast dye injected into the patient's bloodstream. The dye, typically iodine-based, enhances the visibility of blood vessels by absorbing X-rays and appearing as bright areas on the CT images. This contrast enhancement is crucial for distinguishing blood vessels from surrounding tissues and organs, facilitating accurate interpretation of the images.
Despite its effectiveness, CTA does come with certain considerations. One notable aspect is the exposure to ionizing radiation associated with X-rays. While modern CT scanners employ dose-reduction techniques to minimize radiation exposure, healthcare providers must weigh the benefits of the procedure against the potential risks, especially for patients who may require repeated imaging studies.
Another consideration is the use of contrast dye, which can have implications for patients with kidney problems or allergies to iodine-based substances. Special precautions, such as pre-screening for kidney function and administering alternative contrast agents, may be necessary to ensure the safety of these patients during CTA.
In clinical practice, CTA finds widespread use in various medical specialties, including cardiology, neurology, vascular surgery, and radiology. It plays a crucial role in diagnosing conditions such as coronary artery disease, pulmonary embolism, aortic aneurysms, peripheral arterial disease, and intracranial vascular disorders.
MRI Angiography (MRA): Harnessing the Power of Magnetic Resonance Imaging

In contrast to CTA, MRI Angiography (MRA) utilizes magnetic resonance imaging technology to visualize blood vessels without the use of ionizing radiation. This non-invasive imaging technique relies on the interaction between strong magnetic fields and radio waves to create detailed images of the vascular system.
The process of MRA begins with the patient lying comfortably on a table that moves into the MRI machine. Inside the MRI scanner, the patient's body is exposed to a powerful magnetic field, aligning the hydrogen atoms in the body's tissues. Radio waves are then emitted, causing these aligned atoms to produce signals that are detected by the MRI machine and converted into images.
One of the primary advantages of MRA is its safety profile in terms of radiation exposure. Since it does not use X-rays or ionizing radiation, MRA is considered a preferred imaging modality for patients who may be sensitive to radiation, such as pregnant women, children, and individuals requiring repeated imaging studies.
Additionally, MRA excels in producing detailed 3D images of blood vessels, providing valuable insights into blood flow dynamics, vessel morphology, and tissue perfusion. This level of anatomical and functional information is particularly beneficial for evaluating conditions such as cerebral aneurysms, vascular malformations, stroke, renal artery stenosis, and peripheral vascular disease.
Despite its advantages, MRA does have certain considerations and limitations. MRI machines can be noisy during operation, which may cause discomfort or anxiety for some patients. Furthermore, patients with certain medical implants or devices, such as pacemakers, cochlear implants, or metallic objects, may not be eligible for MRI scans due to safety concerns related to the magnetic field.
In clinical practice, MRA is widely utilized across various medical specialties, including neurology, cardiology, vascular surgery, and orthopedics. It is instrumental in diagnosing and monitoring vascular disorders, guiding surgical interventions, and assessing treatment outcomes.
Here's a table summarizing the key differences between CT Angiography(CTA) and MRI Angiography (MRA):
Aspect | CT Angiography (CTA) | MRI Angiography (MRA) |
Technology | X-rays and contrast dye | Magnetic fields and radio waves |
Radiation Exposure | Ionizing radiation | No ionizing radiation |
Image Quality | High-resolution, 3D | Detailed, soft tissue contrast, 3D |
Contrast Agents | Requires iodine-based contrast dye | May or may not use contrast agents |
Safety Considerations | Radiation exposure, contrast dye implications | No radiation exposure, limitations for certain medical implants |
Clinical Applications | Coronary artery disease, pulmonary embolism, aortic aneurysms | Cerebral vascular disorders, stroke, peripheral vascular disease |
This table provides a concise comparison of the essential differences between CTA and MRA in terms of technology, safety, image quality, contrast agents, and clinical applications.
While both CTA and MRA serve the purpose of visualizing blood vessels, they differ significantly in terms of technology, image acquisition, safety profiles, and clinical applications. Understanding these differences is essential for healthcare professionals to select the most appropriate imaging modality based on individual patient needs and diagnostic requirements.
Technology Used:CTA utilizes X-rays and contrast dye, whereas MRA relies on magnetic fields and radio waves.
Radiation Exposure: CTA involves exposure to ionizing radiation, while MRA does not use ionizing radiation and is considered safer in this regard.
Image Quality: Both CTA and MRA can produce high-resolution images, but MRA excels in soft tissue contrast and 3D visualization.
Contrast Agents: CTA requires the use of iodine-based contrast dye, whereas MRA may or may not use contrast agents, depending on the specific imaging protocol.
Safety Considerations: CTA may pose risks related to radiation exposure and contrast dye administration, especially for patients with kidney problems or allergies. MRA is generally safer in terms of radiation exposure but has limitations for patients with certain medical implants or devices.
Clinical Applications: CTA is commonly used in assessing coronary artery disease, pulmonary embolism, aortic aneurysms, and peripheral arterial disease. MRA is preferred for evaluating cerebral vascular disorders, vascular malformations, renal artery stenosis, and soft tissue perfusion.
In summary, both CT Angiography (CTA) and MRI Angiography (MRA) are invaluable tools in modern medicine for visualizing blood vessels and diagnosing vascular conditions. The choice between CTA and MRA depends on factors such as the area of interest, patient characteristics, safety considerations, and diagnostic goals. Healthcare providers must carefully evaluate these factors to ensure optimal patient care and diagnostic accuracy.
In the domain of vascular imaging, CT Angiography (CTA) and MRI Angiography (MRA) stand as pillars of diagnostic excellence, offering clinicians a window into the intricate network of blood vessels within the human body. While CTA harnesses the power of X-rays and contrast dye to create detailed images, MRA leverages magnetic resonance technology for radiation-free visualization. The journey of selecting the most suitable imaging modality involves considerations of patient safety, diagnostic precision, and clinical utility. Healthcare providers must weigh the benefits and limitations of CTA and MRA, aligning them with the unique needs of each patient and the diagnostic challenges presented.
As technology continues to advance, the landscape of vascular imaging is poised for remarkable transformations. Innovations in imaging modalities, such as CT Angiography (CTA) and MRI Angiography (MRA), are driving improvements in diagnostic accuracy, patient safety, and clinical outcomes. Emerging technologies, such as dual-energy CT, contrast-enhanced ultrasound, and advanced MRI sequences, offer enhanced capabilities for visualizing blood vessels with greater precision and detail.
One notable development in vascular imaging is the integration of artificial intelligence (AI) and machine learning algorithms. These AI-driven tools analyze vast amounts of imaging data, enabling automated interpretation, lesion detection, and quantitative assessment of vascular parameters. AI algorithms can aid radiologists and clinicians in making faster and more accurate diagnoses, leading to personalized treatment strategies and improved patient care. Furthermore, the advent of hybrid imaging systems, such as PET/CT and PET/MRI, is revolutionizing the field of vascular medicine. These integrated platforms combine functional imaging (PET) with anatomical imaging (CT or MRI), providing comprehensive insights into both metabolic activity and vascular anatomy. Hybrid imaging is particularly beneficial in oncology, where it helps evaluate tumor vascularity, monitor treatment response, and guide therapeutic interventions.
In parallel, miniaturization and portability of imaging devices are expanding access to vascular imaging in diverse clinical settings. Handheld ultrasound devices, portable CT scanners, and compact MRI systems offer point-of-care imaging capabilities, enabling rapid assessment of vascular emergencies, bedside monitoring, and outpatient imaging services. These portable solutions empower healthcare providers to deliver timely interventions and improve patient outcomes, especially in resource-limited settings or remote areas.
Moreover, advancements in contrast agents and imaging protocols are enhancing the diagnostic value of vascular imaging studies. Novel contrast agents with improved safety profiles and targeted molecular imaging capabilities enable precise delineation of vascular pathology, such as atherosclerotic plaques, thrombi, and aneurysms. Optimized imaging protocols, including time-resolved angiography and functional MRI techniques, provide dynamic information about blood flow patterns, vascular permeability, and tissue perfusion, aiding in the assessment of vascular physiology and pathology.
Looking ahead, the integration of multimodal imaging approaches, including fusion imaging and image fusion algorithms, holds promise for comprehensive vascular assessment. Fusion imaging combines data from different imaging modalities, such as CTA, MRA, ultrasound, and nuclear imaging, to create fused images that synergistically capture structural, functional, and molecular information. This integrated approach enhances diagnostic accuracy, improves treatment planning, and facilitates image-guided interventions for complex vascular conditions.
In conclusion, the evolving landscape of vascular imaging is characterized by continuous innovation, driven by technological advancements and interdisciplinary collaboration. The synergistic integration of advanced imaging modalities, AI-driven analytics, portable devices, contrast agents, and multimodal imaging strategies is reshaping the paradigm of vascular medicine. These transformative developments are poised to enhance diagnostic capabilities, optimize therapeutic outcomes, and ultimately improve the quality of care for patients with vascular disorders.
In embracing these cutting-edge technologies and methodologies, healthcare professionals and researchers are poised not only to revolutionize vascular imaging but also to pave the way for personalized medicine and precision healthcare. As we continue to explore the frontiers of vascular imaging, collaboration across disciplines and ongoing research efforts will be crucial in harnessing the full potential of these innovations. Together, let us navigate this dynamic landscape, unlocking new insights, and shaping a future where every patient receives the best possible care tailored to their unique vascular needs.